When parents learn their child is diagnosed with achondroplasia – the most common form of dwarfism – they soon discover that height is just one of the ways their child could potentially be affected.
“For many parents, the majority of whom are of average height, they recall this as an overwhelming time. They begin to search for information about a condition they’ve often never heard of, and that has some scary potential complications, all while welcoming a new child,” says Stacie Cavallaro, Director of Global Patient Affairs at BioMarin. “And what parents discover is that the height of their child is far from the only thing they need to monitor and stay vigilant about.”
Achondroplasia is a skeletal condition that affects nearly all the bones in the body – which is why the potential impacts can extend far beyond height. The condition stems from a single root cause: a change in the FGFR3 gene, which encodes for the protein fibroblast growth factor receptor 3 (FGFR3). The FGFR3 protein is found on the surface of chondrocytes, cells in the cartilage that line up to form new bone.
“Bone growth involves a complex interplay of molecular signals. Some signals promote bone growth, while others – such as FGFR3 – slow it down,” explains Kevin Eggan, Chief Scientific Officer and Head of Research and Early Development at BioMarin. “The genetic change in achondroplasia produces FGFR3 receptors that are always turned on, so there’s a constant signal telling bone growth to slow down.”
The Impacts of Impaired Bone Growth
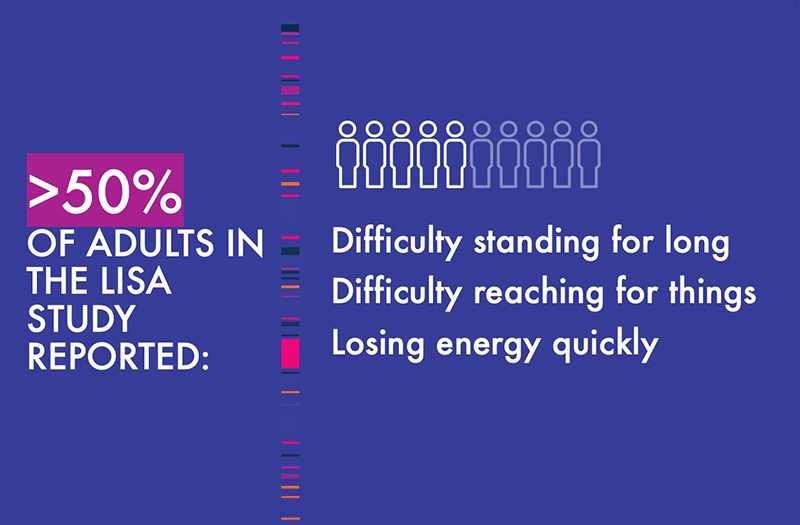
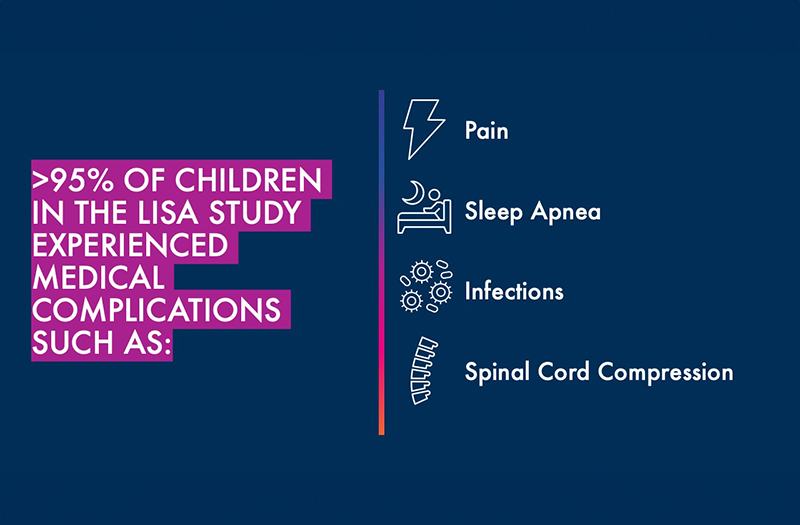
When bone growth is impaired throughout the body, it can lead to a wide variety of complications, ranging from the subtle to the severe. Some of the most common medical complications people with achondroplasia may face are ear infections, sleep apnea, spinal stenosis and pain. In addition, everyday tasks such as reaching, bathing and walking long distances can be difficult.
In rare cases, children with achondroplasia may experience life-threatening complications, including brain stem compression or hydrocephalus (buildup of fluid in the brain).
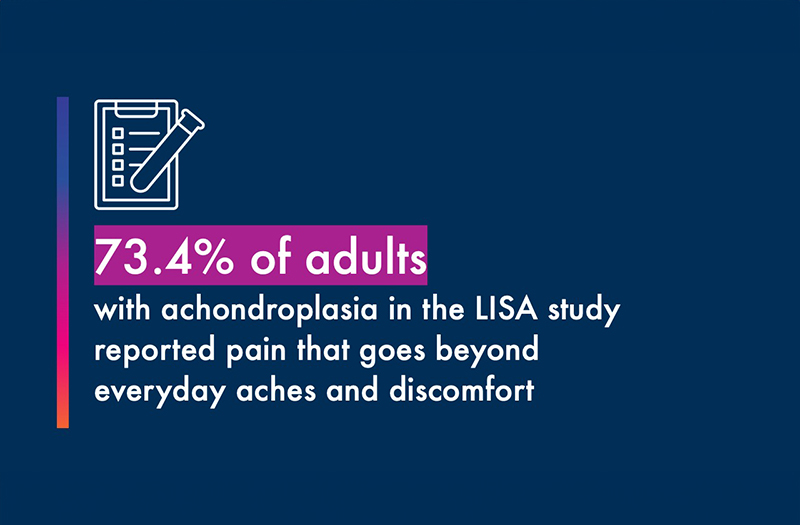
Extensive research is ongoing to deepen collective understanding of the challenges people with achondroplasia face. One recent multinational study conducted by BioMarin, the Lifetime Impact Study for Achondroplasia (LISA), focused on health-related quality of life, with a number of important findings about the range of potential impacts.
“Physical and psychological challenges in achondroplasia can significantly impact a person’s well-being,” says Marcia Kayath, BioMarin’s Senior Vice President and Head of Global Medical Affairs, who began her career as a physician and endocrinologist. “Among the individuals in the LISA study, there were frequent reports of significant pain, lower scores on quality-of-life questionnaires and a high rate of medical complications.”
To better support the achondroplasia community, advocates note that a holistic approach is needed. This includes improving accessibility, increasing psychosocial support and providing options for people seeking treatment, Stacie says.
“From advocating for an experienced care team, to working with schools on creating a conducive and accessible learning environment, having a more comprehensive understanding of the complexities of the physical, mental and social aspects of the condition will ensure parents are properly equipped for what may come next,” she says.
Looking Ahead
Jonathan Day, Group Vice President of Late-Stage Clinical Development at BioMarin, notes that the clinical outlook in achondroplasia is changing with new research and innovation.
“The research we and our partners are leading continues to tell us more about all of the potential impacts of achondroplasia,” says Jonathan Day, Group Vice President of Late-Stage Clinical Development at BioMarin. “We are deeply committed to understanding more about how altered FGFR3 signaling can affect people with achondroplasia and other skeletal conditions, and look forward to learning more about how we can help this community.”
With continued research and a comprehensive approach to clinical management, there is a chance for improved health outcomes and a greater understanding of achondroplasia that goes beyond short stature.
“When parents are armed with information on the totality of achondroplasia beyond just height, they can make the best choices for their child,” says Stacie.



